Welcome to Connections, our new email-based newsletter. To unsubscribe, click the Unsubscribe button in the email you received. To subscribe, send your email address here.
2025 Issue #5: Linked Articles Only
All articles from the Connections newsletter that have a read more link are included on this page. To request the full newsletter, send your email address here.
staying informed: understanding hospice coverage
It is easy to become overwhelmed when reviewing legal or medical documents, including hospice admissions paperwork. Although our Admissions Team works hard to ensure that patients and families understand all that hospice has to offer along with all the regulations involved, it can be helpful to review how it all works.
Understanding Your Coverage When You Elect Seasons Hospice
When you choose Seasons Hospice, our Medical Director reviews the medications, equipment, tests, appointments, and procedures you are currently receiving or have scheduled. Because your goals of care now focus on comfort, symptom relief, and maximizing quality of life, some of your healthcare needs may naturally change.
For example:
You may have taken a cholesterol medication for years to prevent heart disease. At this stage, that medication may no longer provide benefit and could even increase the risk of side effects—so the hospice team may suggest discontinuing it.
Certain lab tests that help manage long-term heart or kidney conditions may no longer be necessary when treatment decisions are guided by your current symptoms.
Many medications meant to prevent problems in the future may not be useful now—and some may carry more risk than benefit. Your hospice nurse, medical director, social worker, and the rest of the team will always include you, your caregiver(s), and/or your representative(s) in these conversations.
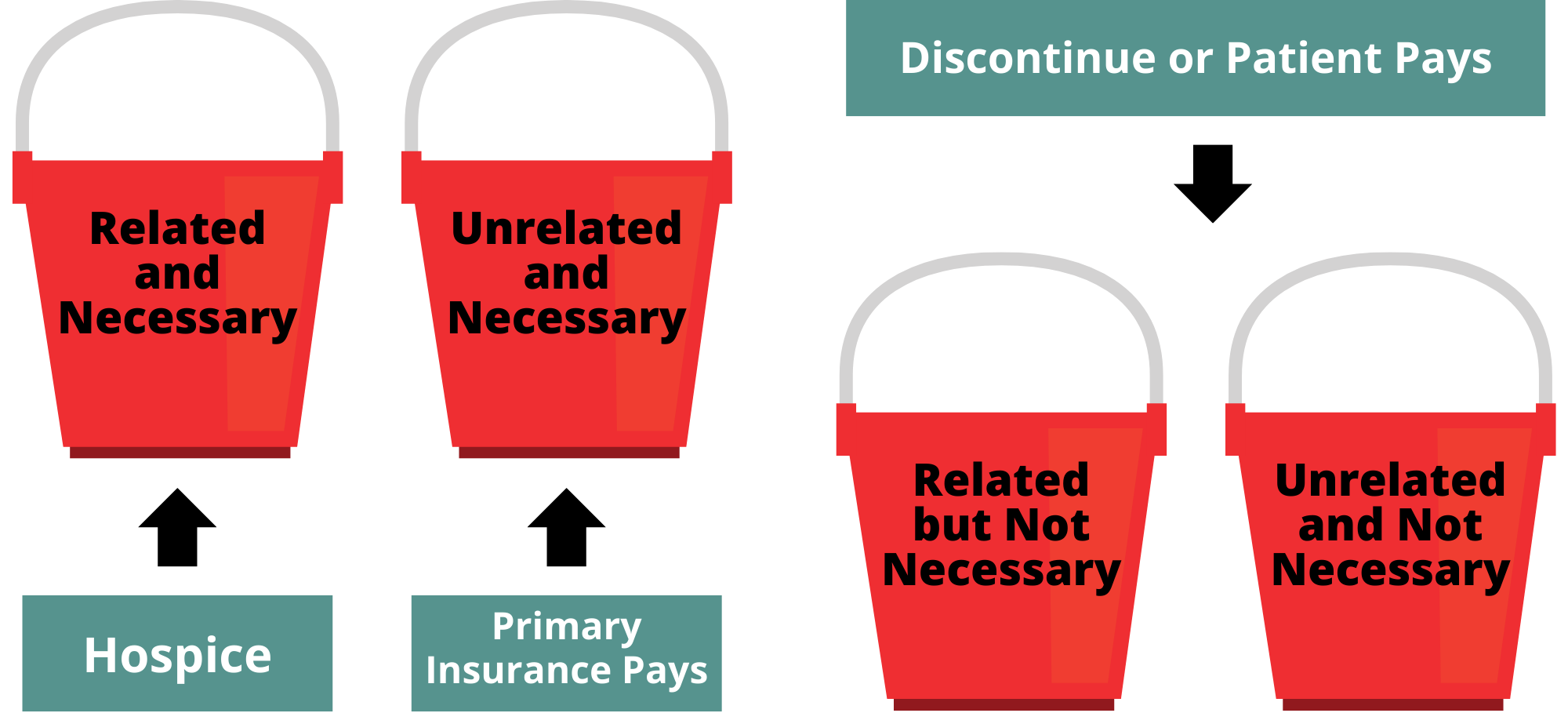
How Seasons Hospice Explains Coverage: The “Bucket Model”
To make coverage decisions easier to understand, Seasons Hospice uses a simple “bucket” model based on Medicare (CMS) guidelines. On your coverage worksheet, our staff will list your medications, equipment, tests, appointments, and procedures under one of four buckets.
Our goals are to:
Make sure your care aligns with your current goals and symptoms.
Highlight anything that might create an out-of-pocket cost.
Help you understand your options and make informed decisions.
We know hospice admission comes with many changes. Coverage discussions will continue throughout your time with us, and we will always explain the reasoning behind any recommendation.
The Four Coverage Buckets
A. Related and Medically Necessary
These services relate directly to the illness you are dying from and affect your prognosis. Hospice covers these services and all medications on our formulary. We also must cover anything needed to manage pain, nausea, constipation, vomiting, or anxiety.
Example: A diuretic used to manage symptoms of heart failure.
B. Unrelated and Medically Necessary
These services address conditions that are not related to your hospice diagnosis and do not affect your prognosis. Hospice does not cover them. Most are paid for by your supplemental insurance or Medicare Part D. We encourage you to check your insurance plan to confirm coverage.
Examples: Eye drops for glaucoma; thyroid replacement medication for hypothyroidism.
C. Related but Not Medically Necessary
These services are related to your condition but, in the Medical Director’s judgment, no longer provide symptom relief or may increase risk. Hospice does not cover non-formulary medications or services that are not medically necessary.
Your team may suggest stopping these treatments or switching to a safer or covered alternative. You may choose to pay privately if you wish to continue them.
Examples: Specialty heart-failure medications, dementia medications aimed at slowing decline, CPAP supplies, specialty COPD inhalers, glucose monitoring systems.
D. Unrelated and Not Medically Necessary
These services are unrelated to your hospice diagnosis and do not provide medical benefit at this stage. Hospice does not cover them.
Examples: Vitamins, herbal supplements, most over-the-counter products.
MEET THE STAFF
This year, we’re excited to give you an inside look at the incredible team behind our hospice care. Each issue of Connections will introduce you to different groups within our staff, showcasing the compassionate individuals who make a difference every day. As the year closes, we want to introduce you to the beating heart of our team: our nurses and aides.
OUR Home Care Team: The Center of All That We Do
Developing a close relationship with the roads of southeast Minnesota is one of the byproducts of being on the Seasons Hospice care team. For our nurses and aides, visiting our patients—wherever they call home—is at the very heart of what they do! They are our patients’ most essential resource. They are the care team leaders, they provide crisis support and a kind shoulder to lean on, always holding you fast in their care and helping ensure a dignified experience during the hospice journey. As one who works closely with the nursing staff, social worker Vanessa shared that, “As their social work partner, I’m constantly grateful for the way our nurses lead with heart, collaborate with care, and honor each person’s story. It’s a privilege to walk alongside them in this work.”
Our registered nurses (RNs), licensed practical nurses (LPNs), and hospice aides, as well as our clinical services manager and resource nurse are dedicated professionals who work diligently to keep patients comfortable in their own homes (wherever that may be) when life-saving treatment is no longer warranted, available, or desired. RN Brittany put it this way, “Instead of you coming into the clinic, the clinic comes to you!” This means that you receive:
Care and treatment in your home
Medication, medical equipment, and other supplies brought to your home
Your needs, in other words, are met at home.
individual roles
The typical RN has their own caseload of patients that they follow throughout their time on hospice in addition to providing coverage for other nurses whenever necessary; our on-call RNs cover evenings and weekends. In addition to the primary focus on comfort, they also manage symptoms, find ways to help patients maintain or improve quality of life, provide emotional support for both the patient and their caregivers, and assess for any additional needs, leading to additional support from hospice aides, social workers, or other Seasons staff.
RNs also provide ongoing education to both the patient and the caregivers. This can include guidance on how to provide daily care for the patient and how to administer medications when Seasons staff are not present. Education also includes discussion of the variety of comfort medications available, especially when helping caregivers understand the philosophy of hospice, which is different from other types of care. The goal in hospice is to provide comfort in the days to come, not for the years ahead.
When a patient’s needs change, RNs have quick access to both our medical director and nurse practitioner, so that they can quickly respond to the changing needs of each patient by implementing new protocols or updating medications.
Our LPNs can provide similar care to our patients, except for the initiation of new treatments. They also make an effort to reinforce the education for caregivers.
Our Hospice Aides help with personal care and develop a rapport with individual patients that makes such activities as bathing, grooming, and dressing a more comfortable process. They also deliver supplies, offer companionship, and provide some light housekeeping, thereby alleviating some of the stress that the family and caregivers may be experiencing.
Transitioning and actively dying
One essential role of the nursing team, in particular the RN, is to advise family members and loved ones as to when the patient may be transitioning and entering the actively dying stage. There is no crystal ball or single signal to identify when someone may die, but there are a number of signs, which when they appear together, will indicate that it is time to both pull in extra resources for patient comfort because things can change quickly and start reaching out family, especially if they do not live nearby.
Our trained staff, who have grown familiar with their patients, will often be able to perceive when transitioning begins. Signs may include:
significantly changing appetite
decreasing cognition
becoming bed bound
falling or another incidents
increasing pain or anxiety
hallucinations, including talking to a deceased loved one
When a patient is actively dying, all disciplines across hospice will make themselves available to be there for the patient and their family. In the last three days of life, we make every effort for a patient to be seen daily by an RN or social worker.
BEHIND THE SCENES
Not all of our nurses are on the front lines. Behind the scenes, several staff provide daily, ongoing support to help those out on the road visiting and caring for patients in up to 30-mile radius around Rochester. Their jobs include, but are not limited to:
writing medication orders to pharmacies
triaging phone calls from patients, families, facilities, and pharmacies when nurses are with other patients
responding to any or all needs of nurses and social workers when they are with their patients
providing pharmacy support
providing tech support for field staff using:
* our electronic medical records software
* other staff apps
* equipmentencouraging prompt completion and submission of charting (required in order to bill Medicare)
encouraging staff to follow all quality and compliance rules and regulations
continuous education of staff and onboarding of new employees
They also provide any necessary monitoring and support during a Continuous Care episode in which a patient is receiving direct care by two to three staff to manage severe symptoms, with up to another 10 staff online.
INDEPENENCE & Teamwork
Hospice is about building relationships and getting to know your patient. It is a special time, and our team believes it is an honor to care for people at the end of life and make them comfortable. There is also a level of independence afforded nurses in hospice that gives them a fairly wide scope, as they organize their day-to-day traveling to patients, manage their schedules, plan for re-certifications (which RNs perform at the first two hospice benefit periods), and anticipate patient needs.
RN Anne summed up the experience of working in hospice: “The hospice team is special. The team really has each other’s backs. When another caregiver sees your patient, they will address everything they see and not wait for your next visit to follow up.”
Whether in the office or driving miles every day, our nurses and aides put the comfort, dignity, and quality of life of our patients above all else, and we are so very proud of their dedication.
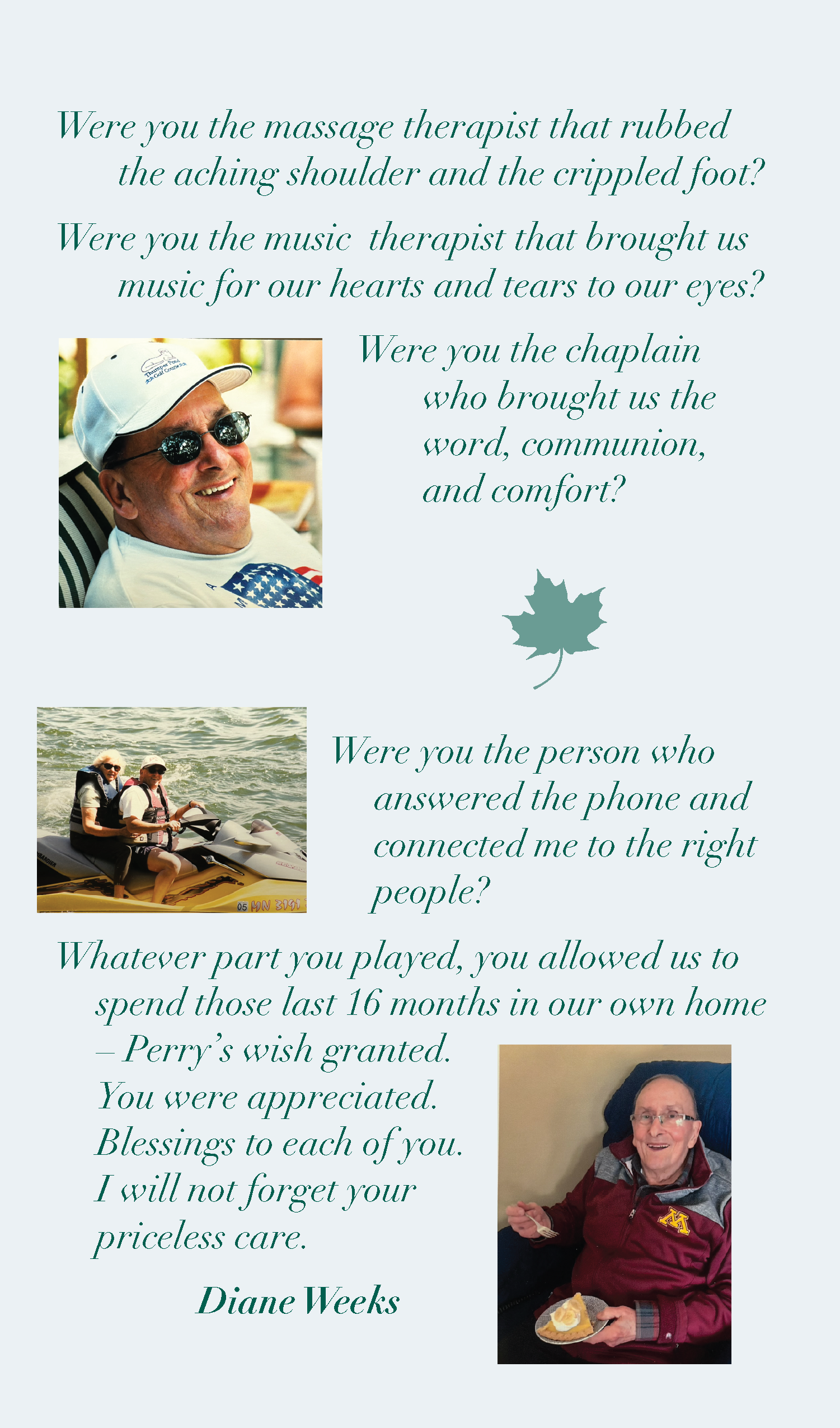
AN ODE TO HOSPICE
PET THERAPY TEAM OF THE SEASON:
Barb & NIGEL
(continued)
Nowadays, Nigel and Barb visit with Seasons’ patients in various types of senior living facilities. Sometimes it can get a bit awkward because for most of his working years, he’s been a bit too heavy to get on a patient’s bed (the limit is 50 lb) but his short legs prevent him from being easily reached by a bed bound patient. So, Barb to the rescue! She sits Nigel on a chair close to the bed so Nigel and the patient can interact. However, having shed a few pounds as he has aged, and now at 48 lb, Nigel is allowed up. In addition to Seasons, Nigel and Barb also visit the campus of the University of Minnesota-Rochester about once a week, and the students get down on the floor with him and let him bring them calm, love, and reassurance.
We also must mention how accomplished Nigel is overall: He has AKC titles in Scentwork (what AKC calls Nosework), Rally, and Therapy Dog! However, sadly (for us), Barb and Nigel are in slow retirement as Nigel reaches the upper age range for his breed. Barb tells us that through good care and responsible breeding, Nigel is doing very well, but that it is time to slow down. We will think about Nigel as he spends his days following the sun around the house, looking for a warm place to nap, or deciding that mom’s lap is actually his favorite place to be.
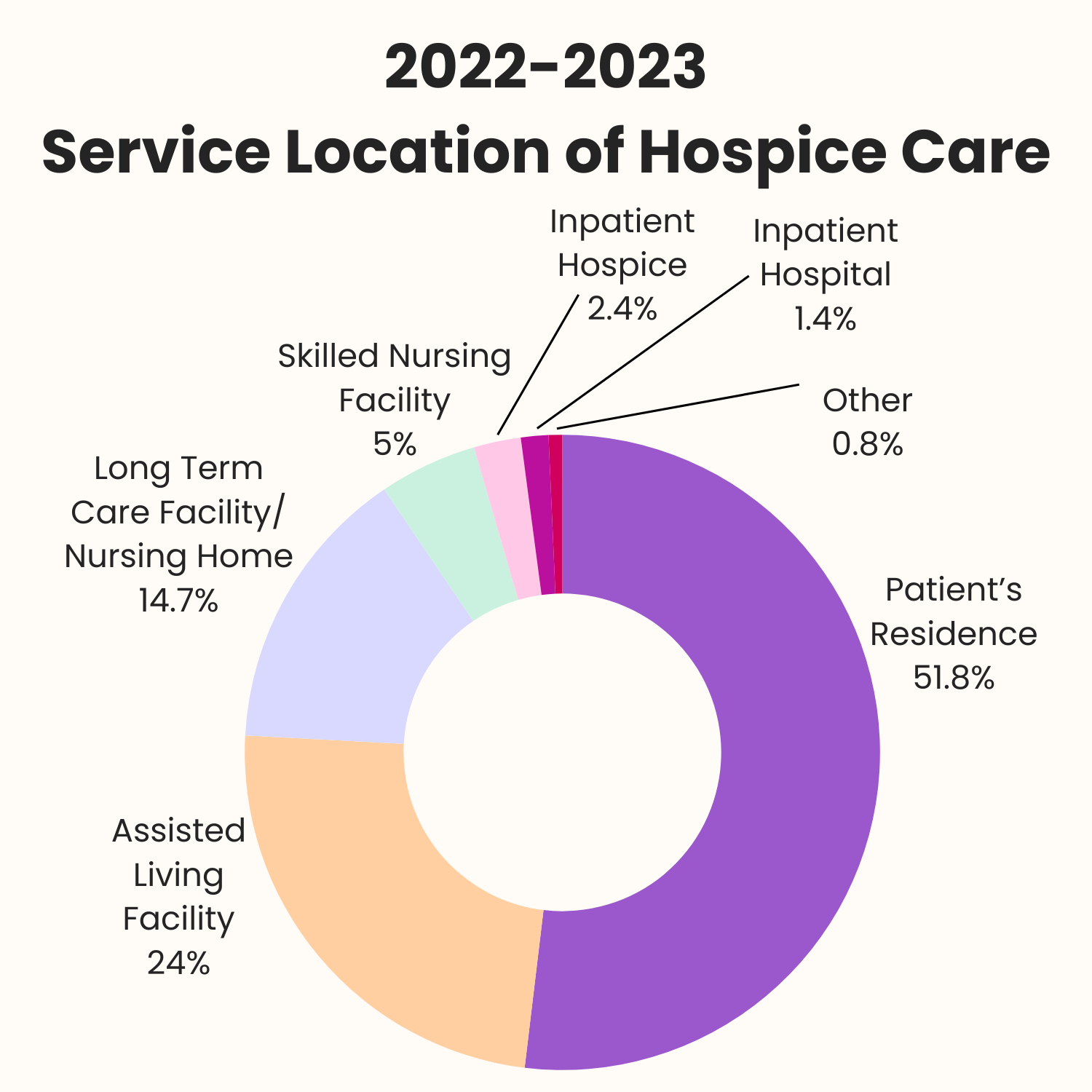
DID YOU KNOW?
HOSPICE FACTS & FIGURES
The Alliance for Care at Home complies a wide range of data regarding the delivery of hospice care in the United States. The chart below represent just a small portion of the data. We will continue to share more data in future issues of Connections.
Source: Hospice Care Chartbook 2024. Research Institute for Home Care. Prepared by KNG Health Consulting, LLC. Sponsored by National Alliance for Care at Home.
NOTES FOR THE JOURNEY:
RESOURCES FOR THOSE NAVIGATING HOSPICE
This month, we offer you the reflection we shared during our recent HopeFULL Holiday programs. Designed to bring joy and companionship to our local assisted living communities, these programs were a joint effort between Seasons Hospice and Home Instead.
Each week, we visited a different community, where we shared a meaningful reflection that encouraged gratitude and hope, led a spirited sing-along featuring classic holiday songs, narrated a heartwarming holiday story, provided treats, and offered comfort from our pet therapy team.